5. Others
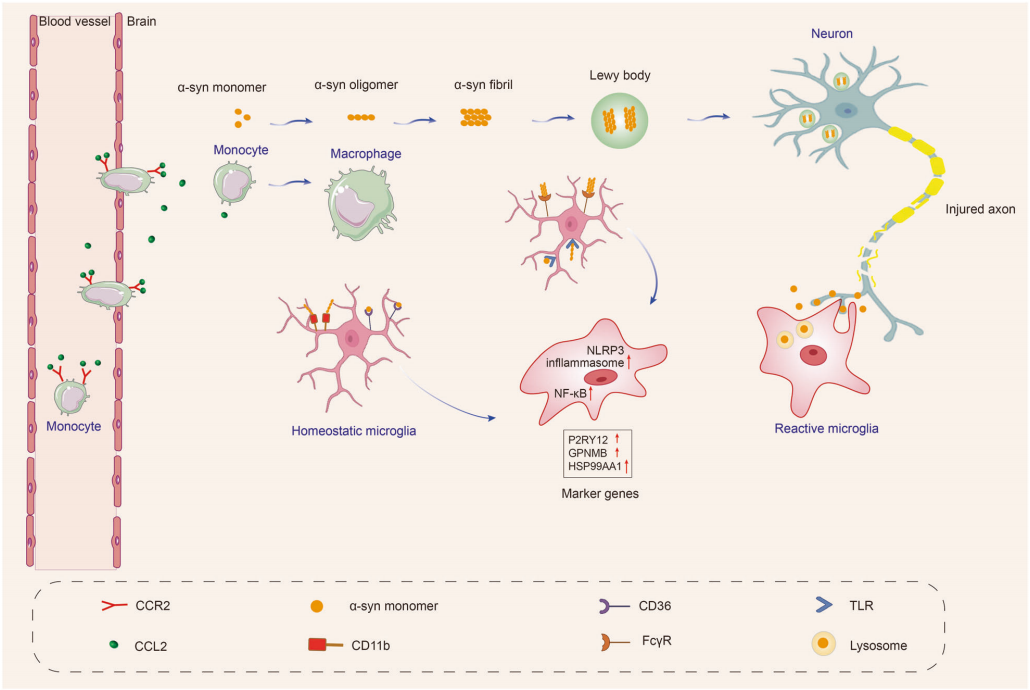
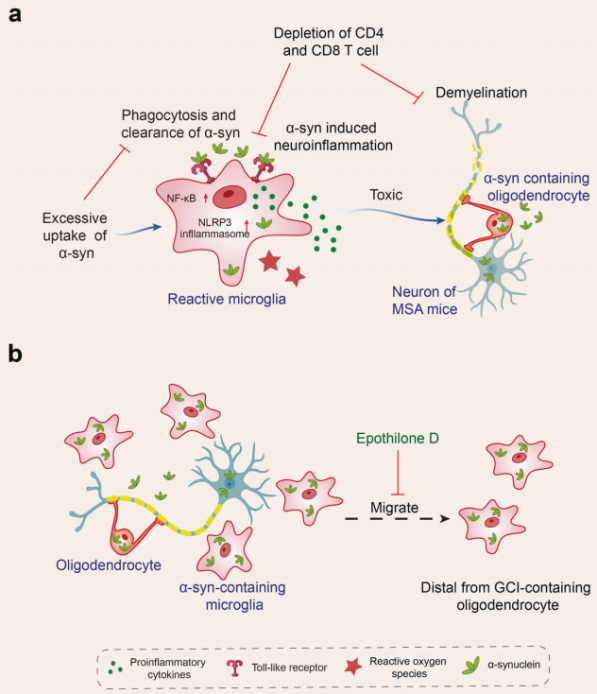
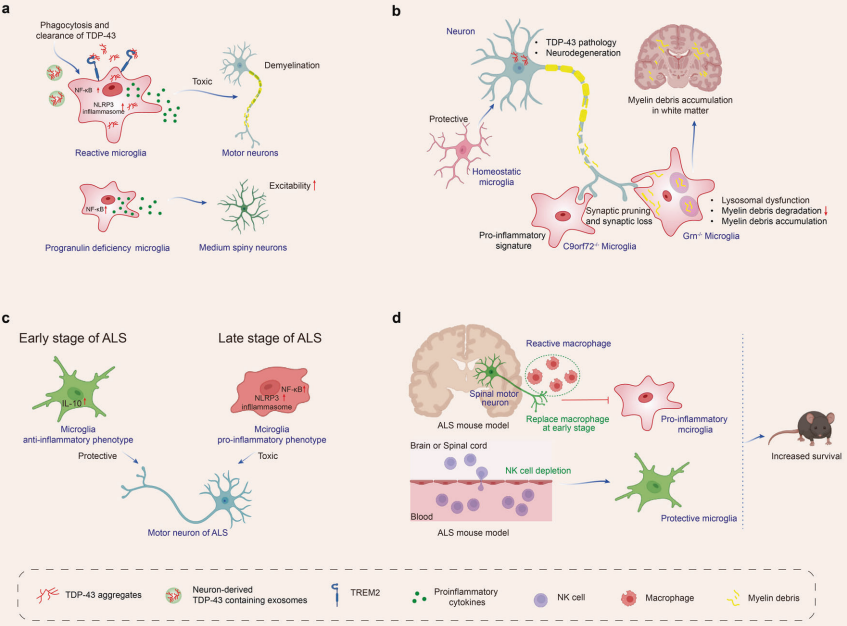
In exploring the relationship between neurodegenerative diseases and microglia, besides the extensively studied diseases such as AD, PD, MSA, ALS, and FTD, progressive supranuclear palsy (PSP), dementia with Lewy bodies (DLB), and Huntington's disease (HD) also demonstrate the crucial role of microglia in disease progression. In PSP, microglial activation is closely related to the accumulation of hyperphosphorylated tau protein (pTau), a process that not only leads to the disruption of microtubule structures and neuronal dysfunction but also promotes the reactive proliferation of microglia and astrocytes, accelerating the process of neurodegeneration. In DLB, the behavior of microglia is similarly complex and variable, transitioning from an early reactive activation state to a later state of atrophy, with phenotypic changes closely linked to the disease stage, accompanied by abnormal aggregation of α-synuclein and coexisting AD-like pathological features. As for HD, microglial activation is closely connected to the abnormal expansion of the CAG repeat sequence in the HTT gene, leading to the misfolding of huntingtin protein and neuronal loss. Multiple signaling pathways, such as NF-κB, kynurenine, and cannabinoid receptor pathways, are involved in this process. Microglia detect and respond to external stimuli through receptors like TLRs, triggering immune responses that further influence disease progression. In summary, the role of microglia in neurodegenerative diseases is multifaceted and complex, with changes in their behavior profoundly impacting the pathological processes and clinical manifestations of these diseases.
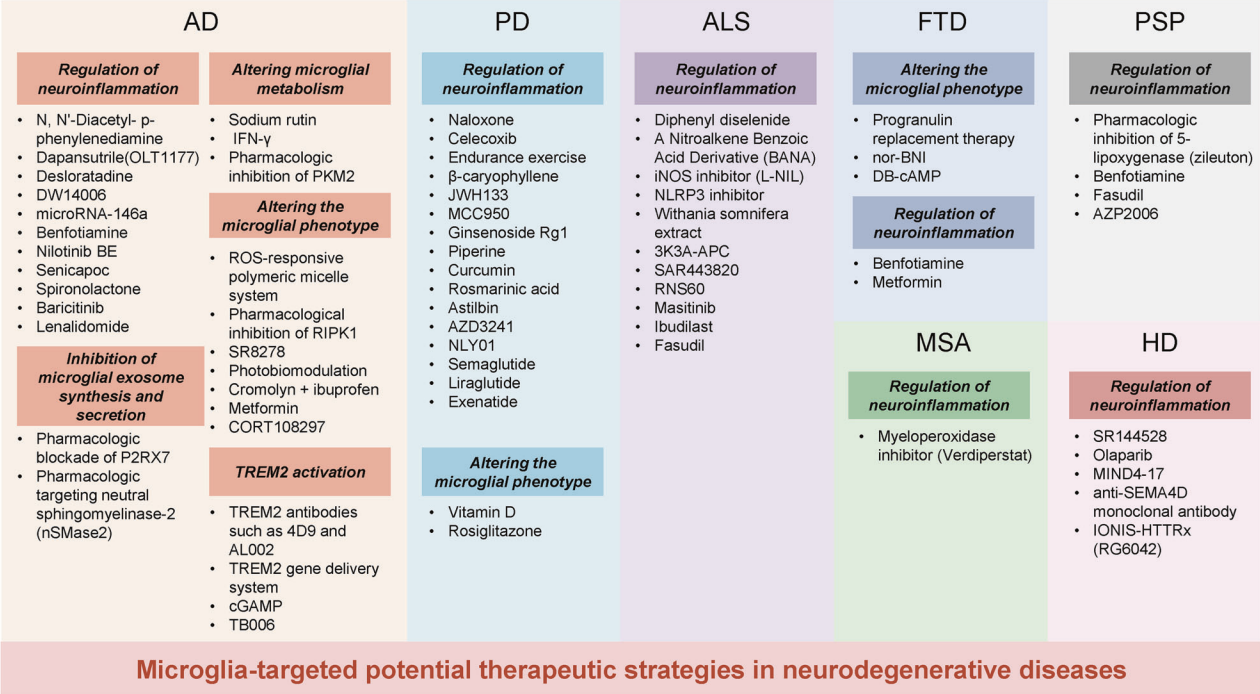
II. Potential Microglial Targeted Interventions and Therapeutic Approaches for Neurodegenerative Diseases
Based on the in-depth understanding of the complex relationship between neurodegenerative diseases and microglia, researchers are actively exploring a range of innovative therapeutic strategies aimed at promoting disease treatment by modulating microglial function. The principles and effects of these strategies have been preliminarily validated in cell experiments, animal models, and clinical trials.
1. Modulating Neuroinflammation
Modulating neuroinflammation is one of the most widely used therapeutic targets, focusing on intervening in the activation state of microglia through drugs or other means to reduce the release of harmful inflammatory factors and thereby alleviate neuronal damage. Research has found that using the NLRP3-specific inhibitor OLT1177 to inhibit the NLRP3 inflammasome can rescue cognitive impairments in AD mouse models. Similarly, the NLRP3 inhibitor MCC950 has been shown to suppress inflammasome activation, α-synuclein aggregation, and dopaminergic degeneration in the substantia nigra of PD mouse models, improving motor function.
2. Inhibiting the Synthesis and Secretion of Microglial Exosomes
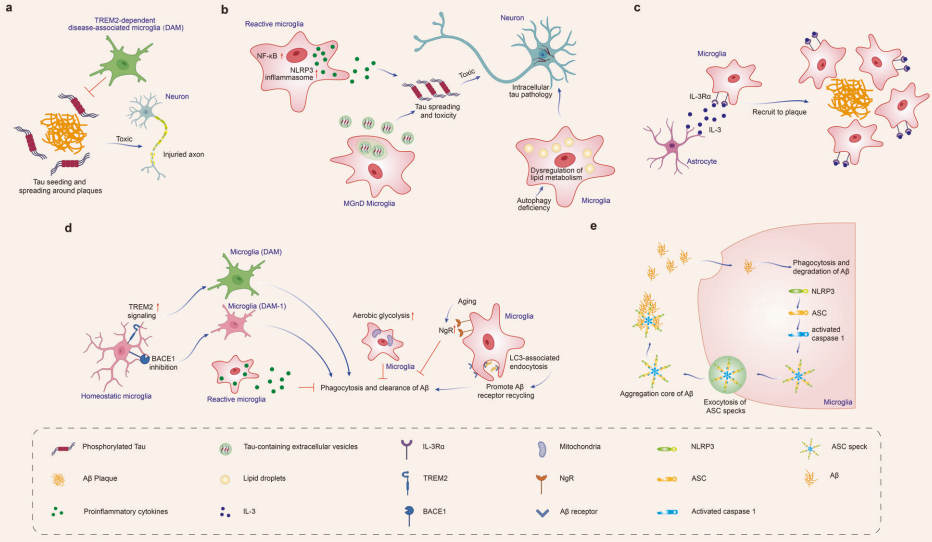
Microglia release exosomes containing tau, and microglial activation can facilitate tau propagation. Inhibiting the synthesis and secretion of microglial exosomes can help reduce tau proliferation. Studies have shown that early pharmacological blockade of P2RX7 in tau mice significantly impairs microglial exosome secretion, reducing tau accumulation in the brain and thereby improving working and learning memory.
3. Modifying Microglial Metabolic Pathways
Microglial phagocytosis requires substantial energy. When microglia switch their metabolism from oxidative phosphorylation to aerobic glycolysis, sustained aerobic glycolysis can impair their immune function. Research indicates that modulating microglial metabolism can enhance their phagocytic capacity for Aβ. For instance, treatment with sodium rutin (NaR) shifts microglial metabolism from anaerobic glycolysis to mitochondrial oxidative phosphorylation, providing sufficient ATP for Aβ clearance. Additionally, NaR promotes the clearance of Aβ by increasing the expression levels of phagocytosis-related receptors in microglia.
4. Changing Microglial Phenotype
The brain microenvironment can regulate the phenotypic transformation of microglia, promoting their positive functions. In AD, a ROS-responsive polymer micelle system can accumulate in lesioned areas by mimicking Aβ transport pathways. These micelles normalize the oxidative and inflammatory microenvironment, promoting microglial regeneration. In PD, vitamin D protects dopaminergic neurons from inflammation and oxidative stress by inhibiting microglial activation and promoting M2 polarization, increasing the expression of M2 microglial markers such as CD163, CD204, and CD206.
5. TREM2 Gene Intervention Activation
Activating the expression of key genes such as TREM2 is also considered to enhance the clearance capacity of microglia, promoting their effective clearance of pathological proteins like Aβ and tau. Studies have shown that enhancing TREM2 signaling through TREM2 agonist antibodies such as 4D9, AL002c, or tetravalent TREM2, or using a gene delivery system targeting microglia to upregulate TREM2 levels in the brain, can enhance Aβ clearance and alleviate neuroinflammation.
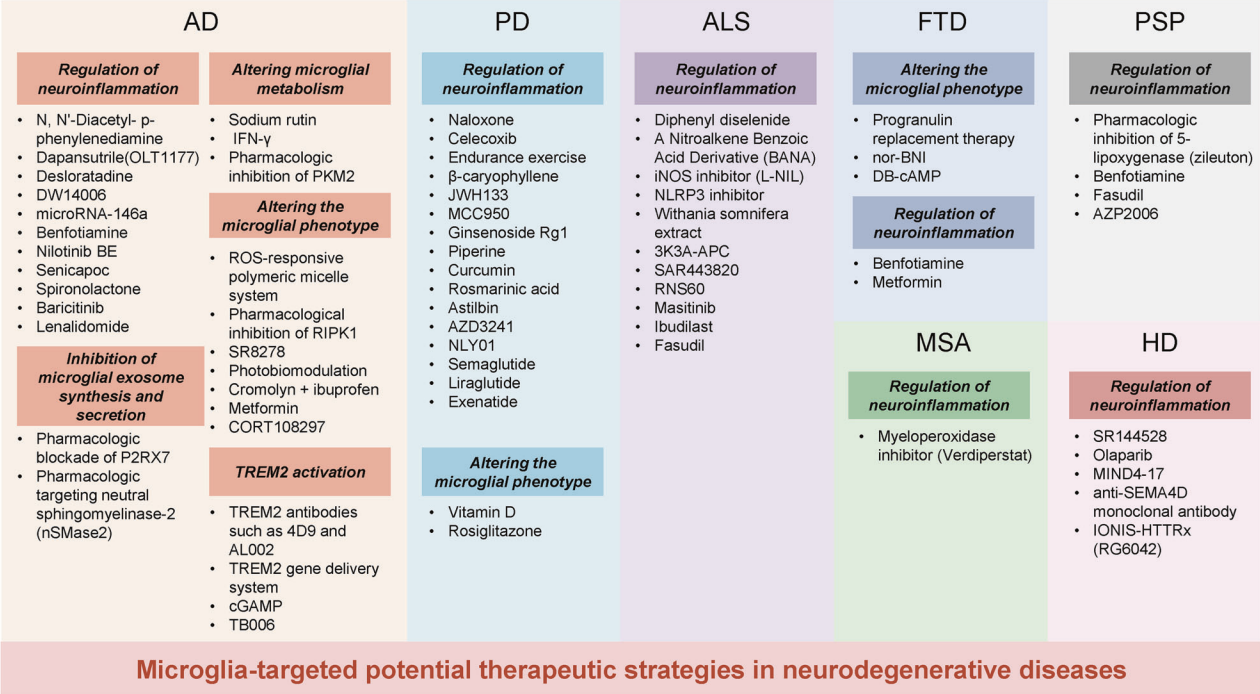
Figure 5: Potential microglial-targeted interventions and therapies for neurodegenerative diseases.
In summary, the role of microglia in neurodegenerative diseases is multifaceted and complex. Through in-depth research and exploration of therapeutic strategies, new insights have been provided for the treatment of neurodegenerative diseases, laying a solid foundation for the future development of more precise and effective therapies.
Brain Case has launched an innovative AAV11 serotype vector, model BC-ZA0182: rAAV-mIBA1-EGFP-WPRE-4×miR-9.T, specifically designed for the efficient and selective transduction of microglia. Furthermore, this vector is flexibly designed to allow for the overexpression or interference of specific genes, or to integrate techniques such as optogenetics, chemogenetics, and calcium signaling recording, thereby providing a powerful genetic manipulation toolset for exploring the functions, mechanisms, and roles of microglia in neurological diseases.
References
Gao C, Jiang J, Tan Y, Chen S. Microglia in neurodegenerative diseases: mechanism and potential therapeutic targets. Signal Transduct Target Ther. 2023 Sep 22;8(1):359. doi: 10.1038/s41392-023-01588-0. PMID: 37735487; PMCID: PMC10514343.